Pth Calcitonin And Vitamin D
Calcium is the fifth most abundant element in the body. It is vital for several biological processes including neurotransmission, muscle contraction, hormone secretion and the clotting cascade. In this article, we will review calcium regulation throughout the body and consider the clinical relevance of this vital element.
Forms of Calcium
The average young adult contains 1200g of calcium in their body, 99% of which is stored in bone, 0.99% in blood and 0.01% inside cells.
Calcium in the blood exists in three forms:
- Free-ionised - diffusible, biologically active.
- Bound to anions e.g. phosphate - diffusible, not biologically active.
- Bound to proteins (mainly albumin) - not diffusible, not biologically active.
Regulation
There are three molecules which regulate the amount of calcium in blood and ensure it is maintained within the normal range. These are calcitriol (vitamin D), parathyroid hormone and calcitonin. The synthesis of calcitriol is completed in the kidneys, p arathyroid hormone (PTH) is secreted by the parathyroid glands, and calcitonin is secreted by the thyroid glands.
Vitamin D
Vitamin D is a long-term regulator of serum calcium, with a half life of around 6 hours. Its main function is to increase the intestinal absorption of calcium.
It can be ingested, or synthesised from a cholesterol precursor as follows:
- 7-dehydrocholesterol is converted into vitamin-D3 under the influence of UV radiation.
- In the liver, vitamin-D3 is converted into 25-hydroxyvitamin-D by 25-hydroxylase. This is relatively inactive.
- In the kidney, 1-α-hydroxylase converts 25-hydroxyvitamin-D into 1,25-dihydroxyvitamin-D, otherwise known as calcitriol. This is metabolically active.
[caption id="attachment_17856" align="aligncenter" width="850"]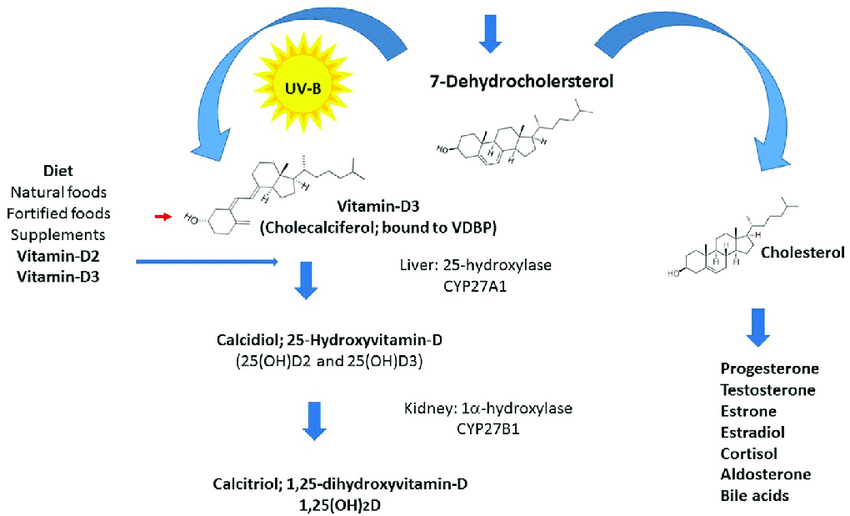 Fig 1 - Schematic diagram of Vitamin D synthesis[/caption]
Fig 1 - Schematic diagram of Vitamin D synthesis[/caption]
Once synthesised, calcitriol is released into the bloodstream. It then stimulates intestinal epithelial cells to increase the synthesis of calbindin-D proteins. Calbindin-D proteins increase the intestinal absorption of calcium by facilitating the transport of calcium from the intestinal brush border to the basolateral membrane, where it is released into the bloodstream.
If levels of calcitriol become excessive, it is converted to 24,25-dihydroxycholecalciferiol, which is less active. This prevents toxicity.
Parathyroid hormone
When the amount of calcium in blood falls below the normal range, inhibition of chief cells in the parathyroid gland is reduced and additional PTH is secreted. PTH raises blood calcium levels by:
- Increasing bone resorption: PTH binds to osteoblasts and upregulates the expression of a protein called RANKL. This stimulates pre-osteoclasts to differentiate into osteoclasts. Osteoclasts resorb bone and release calcium into the bloodstream
- Increasing renal reabsorption of calcium: PTH upregulates the expression of specific channels in the distal convoluted tubule (DCT). This leads toincreased reabsorption of calciuminto the blood, and alsoincreases excretion of phosphate.
- Increasing synthesis of calcitriol:In the kidney,PTH upregulates the expression of 1-α-hydroxylase. This enzyme catalyses the conversion of the relatively inactive 25-hydroxycholecalciferol into calcitriol.
Additionally, PTH and calcitriol inhibit the secretion of PTH from the parathyroid gland. This negative feedback loop ensures blood calcium levels do not continue to rise and go beyond the normal range.
Calcitonin
When the amount of calcium in blood rises above the normal range, parafollicular cells in the thyroid gland secrete calcitonin.
Calcitonin decreases calcium levels by inhibiting osteoclasts, thus reducing bone resorption. Calcitonin has a less significant role in calcium homeostasis than PTH and calcitriol.
[start-clinical]
Clinical Relevance
Hypocalcaemia
Hypocalcaemia is defined as an adjusted calcium level of <2.20mmol/L.
Patients who develop hypocalcaemia acutely tend to be more symptomatic compared to patients who develop hypocalcaemia over a long period of time (chronic hypocalcaemia).
The symptoms of hypocalcaemia include peri-oral and peripheral numbness or tingling, cardiac arrythmias (prolonged QT interval on ECG), muscle spasms, and seizures. This is due to a reduction in the resting membrane potential, rendering the cell hyper-excitable.
Causes of hypocalcaemia include:
- Hypoparathyroidism
- Vitamin D deficiency
- Hyperphosphatemia: Phosphate binds to calcium to form calcium phosphate, reducing free calcium.
- Renal disease:Reduced calcitriol synthesis.
- Acute pancreatitis: Free fatty acids bind calcium, reducing levels of free calcium.
- Respiratory alkalosis: In alkalosis, calcium ions associate with albumin with greater affinity, thus reducing free and active calcium.
Hypercalcaemia
Hypercalcaemia is defined as an adjusted calcium level of >2.60mmol/L.
Patients with mild hypercalcaemia tend to be asymptomatic, but when levels exceed 3mmol/L, symptoms include muscle weakness, cardiac arrhythmias (short QT interval), constipation, kidney stones and depression.
Causes of hypercalcaemia include:
- Hyperparathyroidism
- Malignant tumour - Some tumours secrete parathyroid-hormone related peptide (PTHrP). This mimics PTH, leading to hypercalcaemia.
- Vitamin D intoxication - excess vitamin D causing increased intestinal absorption of calcium.
- Thiazide diuretics - increase renal reabsorption of calcium causing excess calcium in blood.
[end-clinical]
Source: https://teachmephysiology.com/biochemistry/electrolytes/calcium-regulation/

0 Komentar